A Spotlight on the Chronic Pain & Depression Connection this Mental Health Awareness Month
This May marks the 73rd anniversary of National Mental Health Awareness Month—and an opportunity to spotlight the compelling connections between chronic pain and depression.
 At times, pain and depression are so intertwined that it seems impossible to separate one from the other. In fact, studies indicate that one third to three quarters of those suffering from chronic pain also experience moderate to severe depression. Likewise, approximately 65% of patients seeking treatment for depression report at least one type of pain symptom.
At times, pain and depression are so intertwined that it seems impossible to separate one from the other. In fact, studies indicate that one third to three quarters of those suffering from chronic pain also experience moderate to severe depression. Likewise, approximately 65% of patients seeking treatment for depression report at least one type of pain symptom.
The reciprocal cycle of pain and depression can be a devastating one—with pain worsening depression symptoms, and the resulting depression worsening sensations of pain. This unrelenting cycle is particularly palpable in chronic pain patients suffering from fibromyalgia, nerve damage or dysfunction, migraines, osteoarthritis, rheumatoid arthritis as well as chronic back pain. “Chronic pain is exhausting,” says Anodyne of Alpine, Utah Acupuncturist Tricia Corcoran, LAc. Dipl. OM. “And, when a patient has no energy due to pain, they’re not able to engage in the activities they want to, which can, in turn, lead to apathy and the absence of any desire to do anything physical.”
Shared Brain Pathways
Researchers have made great strides in understanding the nuances of how pain and depression impact one another, and why patients often experience pain and depression at the same time.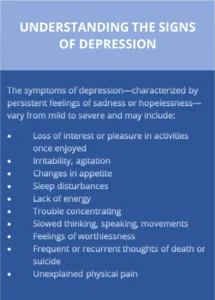
Once upon a time, it was thought that the overlap between pain and depression was mainly a result of psychological factors. Today, thanks to advances in brain and nervous system research, we now know that the connection between pain and depression is more than psychological—it’s also biological.
Researchers have discovered that chronic pain and depression share some of the same nerve pathways in the brain. Specifically, brain pathways that receive pain signals also use some of the same neurotransmitters involved in mood and emotion regulation. When this regulation is disrupted, not only is pain intensified, but feelings of sadness, hopelessness, and anxiety are too. Additionally, some regions of the brain that regulate pain also are involved in the processing and management of emotions and mood. The experience of chronic pain can trigger changes in these brain regions—significantly impacting a patient’s emotional wellbeing.
Holistic Approach
 The intertwined relationship between chronic pain and mental health underscores the value of a comprehensive, multidisciplinary approach to patient wellness—one that addresses the many pieces making up the complex and often challenging mind-body puzzle. “In treating mental health conditions that may be linked to chronic pain, a comprehensive, multidisciplinary approach is especially important because it allows us to provide patients with different ways of increasing neurotransmitter levels,“ says Corcoran. “Acupuncture is a great example of this as studies have shown that it releases both serotonin (our body’s feel-good hormones) and endorphins (our body’s natural pain reliever), which directly impact both depression and pain. In this way, acupuncture can be thought of as a great catalyst for change.”
The intertwined relationship between chronic pain and mental health underscores the value of a comprehensive, multidisciplinary approach to patient wellness—one that addresses the many pieces making up the complex and often challenging mind-body puzzle. “In treating mental health conditions that may be linked to chronic pain, a comprehensive, multidisciplinary approach is especially important because it allows us to provide patients with different ways of increasing neurotransmitter levels,“ says Corcoran. “Acupuncture is a great example of this as studies have shown that it releases both serotonin (our body’s feel-good hormones) and endorphins (our body’s natural pain reliever), which directly impact both depression and pain. In this way, acupuncture can be thought of as a great catalyst for change.”
Below is a sample of other steps patients may take to heal both the mind and body.
- Connect with a therapist: There are several different types of therapies proven to help patients who are suffering from chronic pain and depression. Among these therapies are psychotherapy (what many think of as “talk therapy”) and cognitive behavioral therapy (CBT). CBT helps patients learn how to change negative thoughts, strengthen coping skills, and gain more control over emotions and how pain is experienced.
- Exercise: Physical activity is an amazing mood booster, strengthens the body, and releases endorphins, which are the body’s feel-good neurotransmitters. Aerobic exercise also lowers blood pressure and stress hormone levels, and increases breathing and heart rate, which enables more oxygen to reach cells throughout the body. In turn, this increased flow of oxygen reduces muscle tension.
- Follow an anti-inflammatory diet: Whole grains, nuts, legumes, dark green
- leafy vegetables, and whole fruits (especially berries) are especially effective in controlling pain-inducing inflammation. These foods provide the body with important anti-inflammatory nutrients such as antioxidants, omega 3 fatty acids, polyphenols, prebiotics, and probiotics.
- Practice relaxation techniques: Slow, deep breathing techniques (and related activities such as meditation and yoga) regulate breathing, reduce muscular tension, lower heart rate, and calm the mind.
- Establish good sleep hygiene: Proper sleep restores the body, improves concentration, regulates mood, and improves judgement and decision-making. Without deep sleep, the body is unable to effectively repair and grow tissues. Establish a regular sleep routine that aims for seven – nine hours of sleep a night, with 30 minutes of downtown before bedtime.
At times, the challenges of concurrent chronic pain and depression may feel unsurmountable, but there is hope. If you are experiencing chronic pain or symptoms of depression, we invite you to reach out to an Anodyne provider today. More information about Anodyne’s pain management programs as well as its commitment to patient mental health can be found at https://anodynepain.com.
Related Articles
Whether you’re struggling to diagnose a chronic pain condition or you’re pursuing wellness treatments to stay healthy and feel great, we’re here to support you at every step of your health care journey.
